Spine Surgery Lectures
We have 180 Spine Surgery Lectures in our Spine Surgery Education Programme Diploma. The Spine Surgery Education Programme is endorsed by the European Spine Journal and all our spine surgery lectures are CME Accredited by the EACCME.
24hr Access to all 180 Spine Surgery Lectures
3 CME Credits per Lecture - EACCME Accredited
Ideal for Spine Surgeons & Fellows
Up to 3000 journal articles included
180 World-class online spine lectures
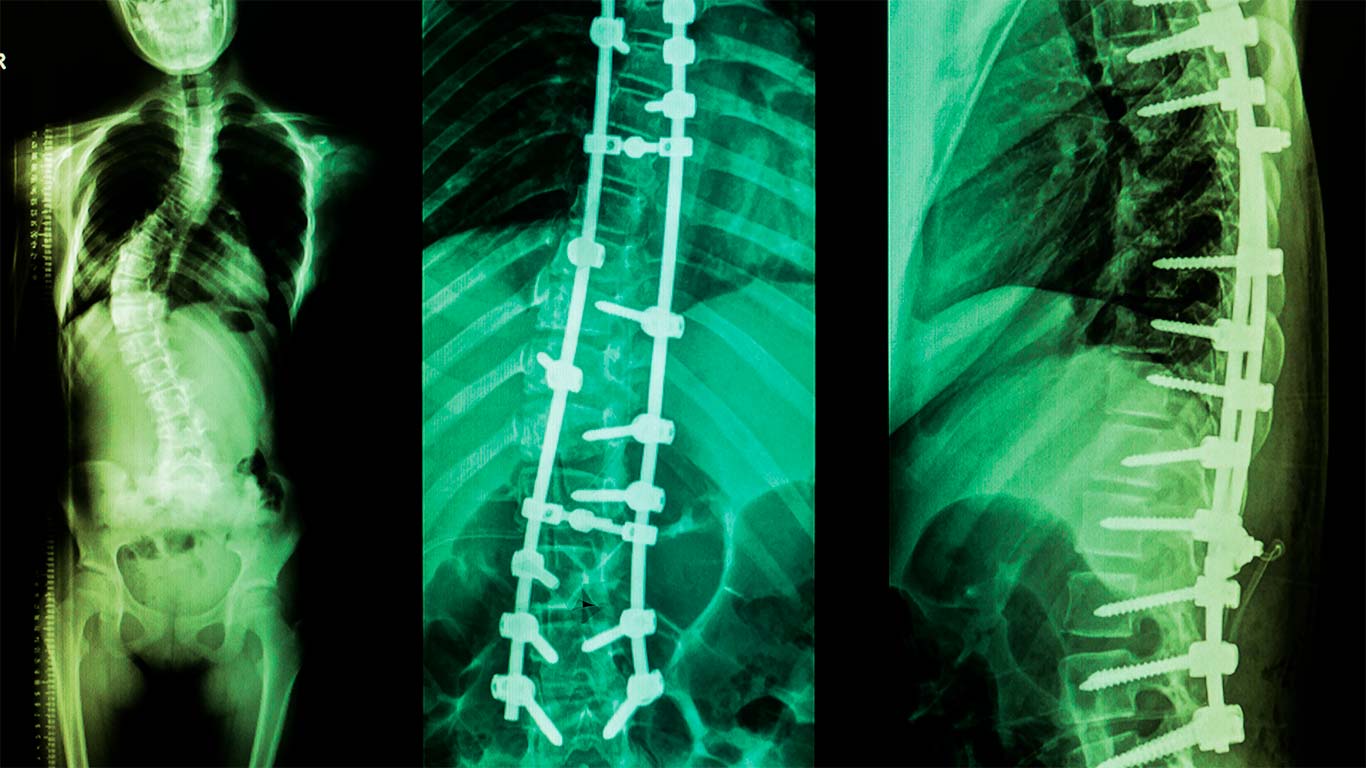
Our 180 spine lectures are grouped by subject in 9 modules, covering all aspects of spine surgery. From Degenerative Disorders to Trauma to Infections, from Biomechanics and Natural History to Operative and Non-Operative Management and Strategies. Browse Lectures.
180 World-class online spine lectures
Our 180 spine lectures are grouped by subject in 9 modules, covering all aspects of spine surgery. From Degenerative Disorders to Trauma to Infections, from Biomechanics and Natural History to Operative and Non-Operative Management and Strategies. Browse Lectures
Learn from over 2000 years of spine surgery experience
Our 130 lecturers have written over 800 book chapters and journal articles on the full range of spine topics. There are founders and editors of spine journals, board members of spine societies, designers of spinal instrumentation used in over 100,000 operations and 33 full Professors. View our full faculty
Learn from over 2000 years of spine surgery experience
Our 130 lecturers have written over 800 book chapters and journal articles on the full range of spine topics. There are founders and editors of spine journals, board members of spine societies, designers of spinal instrumentation used in over 100,000 operations and 33 full Professors. View our full faculty
In-depth spine learning on your time and pace, wherever you are
Our Lectures are online and accessible from anywhere in the world – fit your study around your schedule.
Save time – all relevant materials are available at your fingertips, in context with the relevant slides. Get a comprehensive understanding of a topic without having to do any further research.
In-depth spine learning on your time and pace, wherever you are
Our Lectures are online and accessible from anywhere in the world – fit your study around your schedule.
Save time – all relevant materials are available at your fingertips, in context with the relevant slides. Get a comprehensive understanding of a topic without having to do any further research.
Over 500 hours of additional learning materials
- Over 3000 downloadable journal articles and book chapters*
- 358 Quizzes and assessments
- 16 Surgical Access videos filmed and narrated from the Surgeon’s perspective
* Standard and Premium Course Packages only
Over 500 hours of additional learning materials
- Over 3000 downloadable journal articles and book chapters*
- 358 Quizzes and assessments
- 16 Surgical Access videos filmed and narrated from the Surgeon’s perspective
* Standard and Premium Course Packages only
CME Accredited & Endorsed
Accredited & Endorsed
Testimonials of our Lectures
Our world-class spine faculty
There are over 130 spine experts from around the world in our spine faculty. From Consultant Surgeons to Radiologists, from Professors to Journal Editors, from Physiotherapists to Research Scientists, you get the benefit from their combined 2000 years of experience. See more faculty
Talk to us about our Lectures
Do you have questions or want more information about our Lectures or Spine Courses in general? Just contact us and we’ll get back to you: